U.S. Drug Overdose Deaths More Than Quadrupled from 1999 to 2020
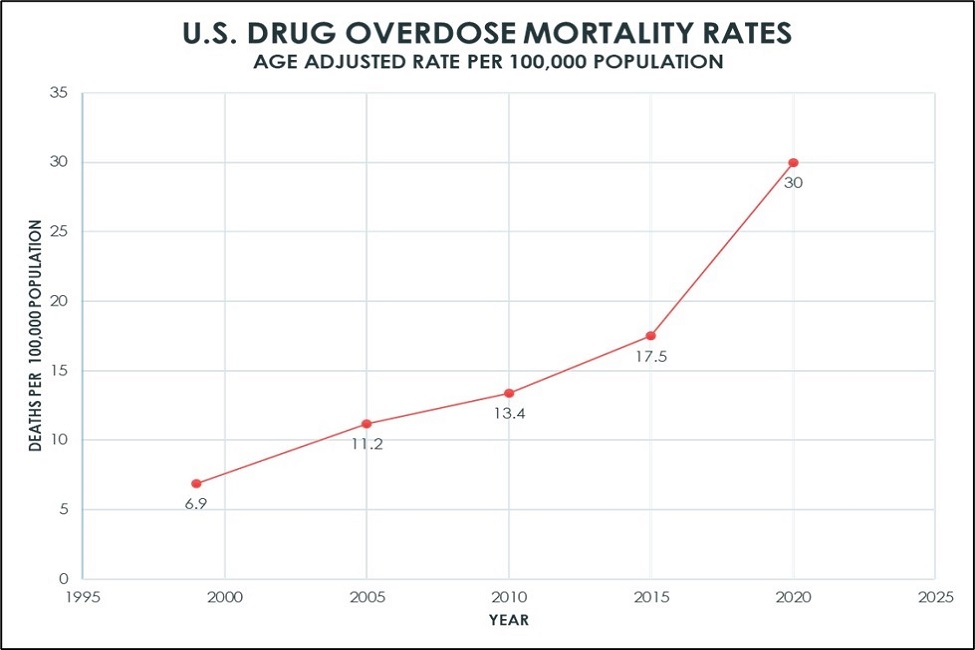
The rates increased 4.4 times from 6.9 per 100,000 in 1999 to 30 per 100,000 in 2020.
The United States is experiencing its highest overall death rates in more than a century, fueled in part by drug overdose mortality. The origins of the current epidemic are due, at least in part, to a 1986 World Health Organization pronouncement that pain treatment is a universal right. As such, cancer pain treatment guidelines were developed, which included the provision of opioids. In 1995, OxyContin was approved for the management of pain, paving the way for widespread prescription of opioids.
Researchers from Florida Atlantic University’s Schmidt College of Medicine and collaborators explored trends in drug overdose deaths in the U.S. from 1999 to 2020, based on age, gender, race, urbanization and geography. Results of their original research, published in The American Journal of Medicine , show that drug overdose deaths in the U.S. more than quadrupled from 1999 to 2020, regardless of race, age, geography or urbanization.
From 1999 to 2020, drug overdoses caused 1,013,852 deaths. The rates increased 4.4 times from 6.9 per 100,000 in 1999 to 30 per 100,000 in 2020. In addition, researchers noted that from May 2022 to May 2023, the U.S. experienced its highest number of drug overdose deaths ever recorded in any 12-month period.
When analyzing subgroups, researchers identified several trends. White and Native Americans or Alaskan Natives have experienced the greatest increase by race. Locations in the Midwest and non-metro areas have been impacted more than other regions.
“Data from our research suggest that clinical and public health interventions should be targeted to populations and regions experiencing the most drug overdose deaths,” said Jennifer Caceres, M.D., senior author and senior associate dean for student affairs and admissions, FAU Schmidt College of Medicine. “Health care providers already have and will continue to play crucial roles in reducing preventable morbidity and mortality from drug overdoses.”
Data from the study show that from 1999 to 2004, Appalachia (primarily West Virginia) and the Southwest (primarily Utah) had the highest death rates from opioids. Over the next five years, mortality rates in these regions increased further and new hotspots appeared in states such as Florida. From 2011 to 2016, hot spots expanded further in Appalachia and the Southwest, but disappeared in Florida, largely due to restrictions on opioid prescriptions. Thereafter, there were marked rises in potentially preventable deaths from heroin.
From 2014 to 2018, fentanyl deaths increased throughout the U.S., although to a lesser extent in the Midwest. Fentanyl has more than 50 times the potency of heroin and 100 times that of morphine. Fentanyl is a synthetic opioid and major cause of drug overdose, especially with the switch from pharmaceutical to illegal forms.
“We believe that guidelines are necessary for guidance, however, health care providers should make individual clinical decisions for each patient and policy makers for the health of the general public,” said Allison Ferris, M.D., second author, chair of the Department of Medicine, and program director of the internal medicine residency program, FAU Schmidt College of Medicine. “To reduce risks of overdose, addiction care should be integrated into the practice of all health care providers regardless of specialty, and training in this area should be further incorporated into medical education.”
The authors note that one immediate challenge is to encourage all providers and state medical societies to ensure the widest distribution and availability of over-the-counter naloxone, an opioid receptor antagonist that rapidly reverses or blocks the effects of opioids, restores normal respiration and heart rhythm, and reverses the potentially fatal effects of an overdose. Earlier this year, the U.S. Food and Drug Administration approved the first over-the-counter forms of Naloxone as either intramuscular such as the EpiPen® or as a nasal spray.
In addition, the authors stress that more focused interventions will better equip health care providers to adequately assess patients for addiction care and assist those patients in gaining access to such care.
“Public health authorities should collaborate with federal, state and judicial systems to treat patients who have drug use disorders in the same way as patients who have a serious chronic disease to avoid premature death,” said Charles H. Hennekens, M.D., Dr.PH, co-author, first Sir Richard Doll Professor of Medicine, senior academic advisor to the dean, FAU Schmidt College of Medicine, and an adjunct professor of family and community medicine at Baylor College of Medicine. “Death is inevitable, but premature death is not.”
The authors conclude that analytic studies designed in advance to do so are necessary to test the many hypotheses formulated from these descriptive data. These include case-control and cohort studies and, where necessary, to reliably detect the most plausible small-to-moderate effects, large scale randomized trials.
For the study, researchers used data from the U.S. Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (WONDER) and Multiple Cause of Death files from the National Center for Health Statistics.
Study co-authors are Tarek Ghaddar, a second-year medical student, FAU Schmidt College of Medicine; Maria Mejia, M.D., an associate professor of family and community medicine, Baylor College of Medicine; Srekar M. Ravi, M.D., an FAU Schmidt College of Medicine graduate and resident in medicine at Mayo Clinic in Phoenix; and Robert S. Levine, M.D., a professor of family and community medicine, Baylor College of Medicine and an affiliate professor of population health and social medicine at FAU-Schmidt College of Medicine.
-FAU-
Tags: faculty and staff | medicine | research