As COVID-19 cases rise and fall at varying rates throughout the world, it’s become clear that the virus affects people and communities in diverse ways, complicating research efforts to fully master its complexity. To discover COVID-19’s impact and further relative research, the university’s Clinical Research Unit (CRU) launched a COVID-19 Registry and Repository through which they collect and store survivors’ stories and blood and saliva samples.
Typically, hospitals collect this kind of information from patients under their care, but many people who had COVID-19 experienced mild symptoms and did not go to the hospital. The CRU Registry and Repository targets this population, collecting data that might otherwise have gone unnoticed. “Most studies recruit in the hospital, whereas we’re reaching out to the community in general. We have people from Miami to Martin County, and about 95% of this cohort didn’t even go to the doctor,” said Ximena Levy, MD, MPH, director of the CRU.
The idea for the Registry and Repository, which opened in August 2020, emerged in the middle of the pandemic as members of the CRU considered what data COVID-19 researchers needed immediately to address gaps in current knowledge and what data they’ll need in the future to answer questions.
Participants make two visits to the Registry and Repository to give samples, take a neurological exam and recount their personal experience of COVID-19.
Each component of the visits yield a different piece of the puzzle. The blood samples provide DNA for genome sequencing, enabling scientists to discover whether there’s a genetic basis behind a person’s ability to recover from COVID-19. The saliva samples will be searched for the presence of biomarkers that indicate disease development. The neurological exam will serve as a benchmark for long-term follow-up. “We’re anticipating a longitudinal study to see if there are longer-term effects neurologically, but we also want to understand the genetic basis for people’s response to the disease. In addition, we want to see if there are biomarkers we can follow during the course of the next several years,” said Gregg Fields, Ph.D., executive director of FAU’s Institute for Human Health and Disease Intervention, which supports the Registry and Repository initiative.
During the interview portion of the visit, participants are asked questions about how they managed their own care, whether they quarantined alone or with family members, and what access they had to the health care system. Participants’ family members may also take part, especially if they quarantined together at close quarters, with a goal that responses will shed light on broader socioeconomic issues relating to health care in South Florida. “It’s different if you quarantine in a seven-bedroom house than if you quarantine in a small apartment with one bedroom. We’re trying to identify disparities and different responses to the disease,” Levy said. “We are also including questions about people’s feelings regarding stigma and discrimination when they tested positive.”
The CRU is continuing to recruit participants for the registry, said Levy, adding that in order to find patterns in the data, they need a large data set. In the meantime, the CRU is unintentionally providing a much-needed service to the community: People really want to talk about their COVID-19 experiences, and the CRU is listening. ⬥
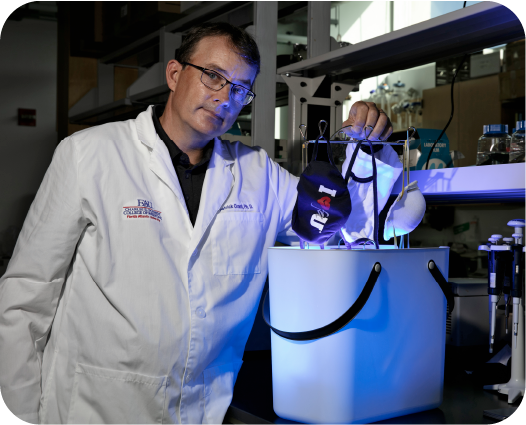
Patrick Grant, Ph.D., associate professor of biomedical science, Charles E. Schmidt College of Medicine, recently designed a new compact and portable sanitizing device for multiple masks that can be used anywhere, on multiple masks simultaneously, keys and smartphones. The device uses ultraviolet light to quickly kill bacteria, yeasts, mold spores and viruses.
Grant’s “portable hanging rack device” comprises an enclosed chamber housed in either a plastic container or steel compartment. Up to six masks can be positioned vertically on an internal rack. The UV light source is shielded within the housing to prevent harm to the user as its radiation deactivates the biological components of the pathogens covering the masks.

A team of researchers in the College of Engineering and Computer Science investigated aerosol droplets generated from flushing a toilet and a urinal in a public restroom under normal ventilation conditions. Aerosol droplets found in public bathrooms are considered the most prominent source of transmission for infectious diseases, including COVID-19, because restrooms are relatively confined, experience heavy foot traffic and may not have adequate ventilation. To measure the droplets, they used a particle counter placed at various heights of the toilet and urinal to capture the size and number of droplets generated upon flushing. They examined the data to determine the increase in aerosol concentration, how high the droplets rose and the impact of covering the toilet. Levels were measured before and after conducting the experiments.
Results of the study, published in the journal Physics of Fluids, demonstrate how public restrooms could serve as hotbeds for airborne disease transmission, especially if they do not have adequate ventilation or if toilets do not have a lid or cover. The study further suggests that incorporating adequate ventilation systems in public restrooms and other spaces would help prevent aerosol accumulation.

To address the needs of widespread testing during the peak of the pandemic, FAU researchers developed a COVID-19 test that is highly accurate and reliable, extracts RNA with commonly available chemicals, uses samples that can be collected at home and can work in pooled samples.
The new test, spearheaded by Massimo Caputi, Ph.D., professor of biomedical science in the Charles E. Schmidt College of Medicine, gets around the global shortage of specific reagents by using TRIzol, a solution used in the extraction of RNA from cells. It is highly sensitive, commonly available and requires minimal biosafety level precautions.
The test works with saliva samples, which can be collected and sent in by the person being tested, reducing person-to-person contact.
What’s more, the test answers a June 2020 call by the U.S. Food and Drug Administration, which encouraged the development of kits that test pooled samples, an approach that originated in the 1980s for testing blood supplies for HIV. The sensitivity of the FAU test makes it a perfect candidate for pooled testing, which enables the high throughput necessary to conduct more than two million tests per day.
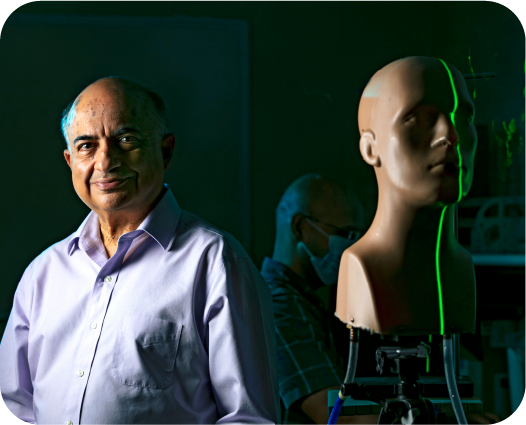
Researchers from the College of Engineering and Computer Science recently received a two-year $698,801 grant from the U.S. Centers for Disease Control and Prevention to test the effectiveness of various types of personal protection measures against airborne viral transmission.
Building on their prior research, the project will result in experimentally verified computational strategies for mitigating airborne transmission of aerosolized droplets for a safe workplace environment.
Researchers will test and quantify the effectiveness of various protective measures under new American Society for Testing Materials standards and best safety practices in the workplace. They will evaluate facemasks and other personal protection equipment; physical safety barriers; interior designs of spaces; air filters, humidifiers; safe seating arrangements in a classroom setting and queuing at checkouts, as well as other measures.
Photography by Alex Dolce